“In the midst of the pandemic, reminders to stay upbeat are everywhere. Mottos, memes and maxims along with Twitter hashtags and Instagram accounts are devoted to preaching optimism as an approach to manage the epic uncertainty. But for some people, the relentless focus on the bright side can go too far.”
This is a quote from an article entitled “It’s OK not to be OK” by Kevyn Burger of the Star Tribune in Minnesota. At the Virtual FA Family Meeting, Dr. Megan Voss shared Burger’s article and shared how the current cultural pressure to maintain an upbeat and positive outlook in the face of a health crisis is 1) nothing new to FA families; and 2) can actually be detrimental to one’s wellbeing. This phenomenon is known as toxic positivity.
What is toxic positivity?
Toxic positivity is the excess and ineffective overgeneralization of a happy, optimistic state across all situations. This results in denial, minimization, and invalidation of the authentic human emotional experience.
We see manifestations of toxic positivity around us all the time. #Blessed. #Thankful. #Grateful. It’s the oversimplified message that it will all be okay if we just put on a smile and get through another day. As individuals who face challenges every day, these messages – even if well-intentioned – are rarely ever helpful.

How do you know if you are experiencing toxic positivity?
- You feel that you have to hide or mask your true feelings
- You try to just ‘get on with it’ by dismissing an emotion
- You feel guilty about what you feel
- Your experiences are minimized with ‘feel good’ quotes or statements
- Perspectives like ‘it could be worse’ are embraced, instead of validating an emotional experience
- You feel shamed or chastised for expressing frustration or anything other than positivity
- Things that bother you are brushed off with an “it is what it is” type attitude
What are the consequences of toxic positivity?
Shame
When in shame, you feel like you have two choices: to be brave or to pretend everything is great all the time. According to leading shame researcher Brené Brown, shame is defined as the intensely painful feeling or experience of believing that we are flawed and therefore unworthy of love and belonging – something we’ve experienced, done, or failed to do makes us unworthy of connection. Brown asserts that shame is neither helpful nor productive, and in fact, is much more likely to be the source of destructive, hurtful behavior than the solution or cure. Guilt and shame are often confused, but unlike guilt, which can be reflective and suggest a change in behavior, shame does not result in positive change.
Suppressed emotions
Studies have shown that people experience less of the physiological signs of stress in the body when they are allowed to outwardly express their emotions. This can happen through words, facial expressions, or tears. If you cry or yell or express what feels bad or sad in a situation, you’re doing your body good by getting that stress out of the body. On the contrary, if you don’t express what you’re truly feeling, and you’re holding back words or tears, you’re housing that stress in your body body, which can lead to negative effects on your health.
Isolation and other relationship problems
If you aren’t free to express yourself, to be seen, to be heard, it’s impossible to relate to others. Research has shown that isolation is detrimental to health and wellbeing. There is an increased risk of developing coronary heart disease and stroke, dementia, and depression.
So, how can we safely combat isolation, especially now when many of us are in lockdown?
- Find safe ways to connect using technology, barriers, and distance. In areas where it’s safe to socially distance outside, connect with people in. your community.
- Reach out to your health care team.
- Utilize telehealth. It’s come a long way and your healthcare providers are here for you.
- Find meaning and purpose in this time of increased isolation. It doesn’t have to be a new hobby or job; it could be spending more time cooking or playing games with your family.
What can I do for myself and my family?
Dr. Voss’ advice for FA families during this time is to:
- Stay safe
- Work with your health care team
- Seek support for not only your physical health, but your mental and emotional wellbeing
- Recalibrate, reassess, refocus. Listening to your body and emotions is the most important part of taking care of yourself.
- Speak up when something doesn’t feel right
- Seek support within your communities that “get it”. The rest of the world may not be able to understand what it’s like to live with FA and now a global pandemic, but other FA families share similar experiences. Reach out in the FA Family Support Group on Facebook (or we can post your concern or question anonymously) or contact FARF Family Services Director Jordan Deines to talk about ways to get connected.
Remember: positivity needn’t be toxic
Cultivating a positive outlook can boost immunity, decrease stress, and even lengthen life spans (Burger). So, how do we embrace positivity but not end up spreading it in a toxic way to others or to ourselves?
- Cultivate real and genuine reasons to feel positive.
- Find the good in the situation. Finding positivity does not have to be this outward expression of joy, like jumping up and down. Everyone has different ways of feeling joy or ‘good’. Remember that the labels of good and bad are subjective, so find what feels right for you.
- Cultivate gratitude and have an active gratitude practice. Our brains are hardwired for negativity, and gratitude is the antidote to that. It takes about 3-4 ‘gratitudes’ or good things to combat a negative thought in our brains. You could do this by going around the dinner table each night, writing them down on slips of paper and into a gratitude jar then sharing them later, keeping a gratitude journal, or even just typing it into the notes tab on your phone. There’s no right or wrong way to keep track of your gratitude, but the key is to be consistent in your practice.
- DO NOT deny yourself negative feelings. Cultivating a positive outlook should never involve denying negative feelings. If you’re feeling anger, sadness or grief, it’s often hard to sit still with those feelings. Sometimes doing something movement-based (exercise, gardening, etc) or creativity-based (art, music, etc.) helps us to express those feelings and allows them to pass.
- Notice any feeling you have and allow it, listen to it, working with it, and through it. Part of mindfulness is simply noticing a feeling, without placing judgment (good or bad) on that feeling.
You’re not expected to not feel sad or to just bounce out of an off mood. As Mary Jo Kreitzer, University of Minnesota, Bakken Center for Spirituality & Healing, reminds us: “Someone who is experiencing overwhelming feelings of sadness can’t flip a switch or jolly their own way out of it. Toxic positivity refuses to acknowledge their challenges. If we ask others to be inauthentic, that doesn’t build resiliency and relationships.”
Tips on what to say & avoiding toxic positivity
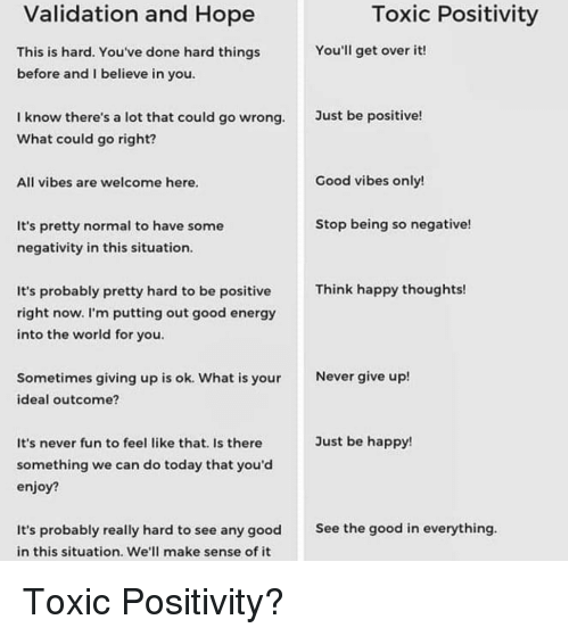
If you or someone you know is struggling, looking on the bright side may not be helpful. Trying to reason away negative feelings or demanding that you “Snap out of it!” likely won’t do any good and may, in fact, be harmful.
Instead, when someone expresses their emotions, listen, then acknowledge and validate their feelings. Instead of assuring them that everything will be OK, say, “I’m here for you, I care for you,” and ask how you can support them.
If someone feels overwhelmed, give them space to talk about their experience without judgment. You can say, “That sounds hard for you, tell me more about that.” Don’t tell them what you would do or feel in their place. Instead, ask them if they just need to vent or want advice.
If the negative feelings deepen or linger, don’t play therapist. People with persistent depressive feelings should be encouraged to see a physician and a mental health professional.